The healthcare landscape is constantly evolving, with a growing emphasis on patient-centered care and improved outcomes. Hospitals are under increasing pressure to enhance their practices, particularly concerning the transition of patients from inpatient to outpatient settings. This focus is driven by the critical need to reduce 30-day readmission rates, prevent adverse events, and ensure a seamless and safe transition for patients returning home or to other care facilities. While transitional care has gained significant attention, understanding what constitutes an effective program is crucial for healthcare providers and institutions aiming to excel in patient care and meet modern healthcare demands.
This article delves into the concept of transitional care programs, exploring their definition, importance, key strategies, and implementation. We will examine successful models and provide insights into how these programs can be effectively implemented to improve patient safety across the continuum of care, with a particular lens on the needs of patients with complex conditions such as neurological disorders.
Understanding Transitional Care Programs: Definitions and Key Components
Transitional care refers to the coordinated set of actions designed to ensure the safe and effective transfer of patients between different healthcare settings, levels of care, or home. A transitional care program is a structured, comprehensive approach to bridge the gaps in care that often occur when patients move from one healthcare environment to another, most commonly from a hospital to their home or another post-acute care facility. These programs are designed to be proactive and patient-centered, addressing the unique needs of individuals during these vulnerable periods.
At its core, a transitional care program aims to create a “bridge” between inpatient and outpatient care. This bridge is built upon several key components:
- Predischarge Planning: This involves starting the transition process while the patient is still in the hospital. It includes assessing the patient’s needs, risks, and resources, and developing a personalized discharge plan.
- Patient and Caregiver Education: Empowering patients and their caregivers with the knowledge and skills they need to manage their health at home is paramount. This includes medication management, understanding warning signs, and knowing when and how to seek help.
- Medication Reconciliation: Ensuring an accurate and complete list of medications and addressing any discrepancies is crucial to prevent adverse drug events, a common cause of post-discharge complications.
- Communication and Coordination: Facilitating clear and timely communication between hospital staff, patients, caregivers, and outpatient providers (primary care physicians, specialists, home health agencies, etc.) is essential for continuity of care.
- Postdischarge Follow-up: Extending support beyond hospital discharge is vital. This can include phone calls, home visits, or facilitated clinic appointments to monitor the patient’s progress, address any emerging issues, and reinforce the discharge plan.
- Dedicated Transition Provider: Often, successful programs involve a dedicated professional, such as a nurse, social worker, or pharmacist, who acts as a point of contact and care coordinator throughout the transition process. This individual “bridges” the gap by providing consistent support and guidance.
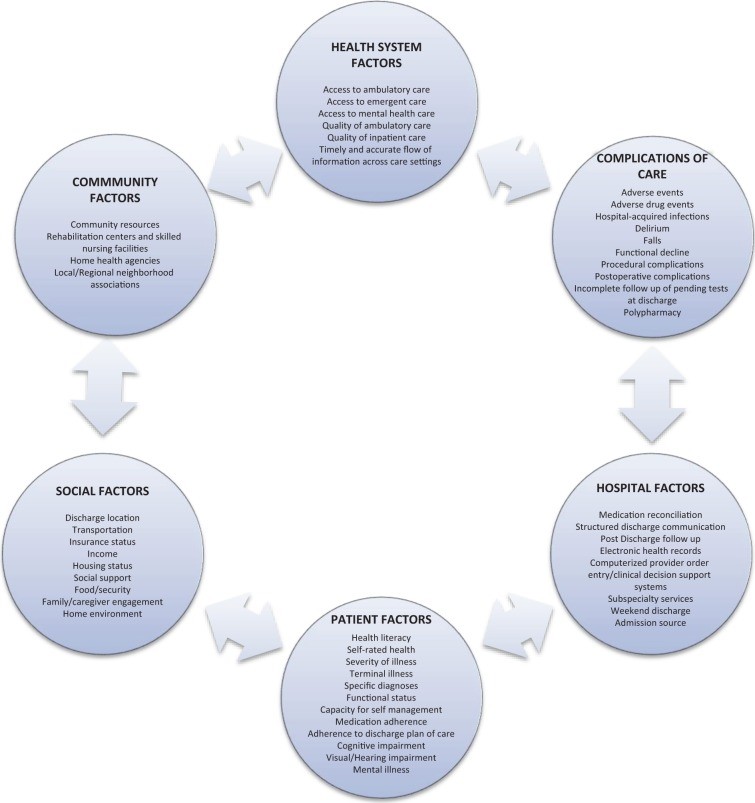 Factors involved in hospital readmission
Factors involved in hospital readmission
Figure 1. Key factors influencing hospital readmission rates. Effective transitional care programs aim to mitigate these risks by addressing patient-specific, system-related, and socioeconomic determinants.
Why are Transitional Care Programs Essential? Addressing the Risks of Poor Transitions
The period immediately following hospital discharge is a particularly risky time for patients. Studies show that a significant proportion of patients experience adverse events within weeks of leaving the hospital, including adverse drug events, hospital-related complications, and new or worsening symptoms. Alarmingly, a substantial number of older adults are readmitted to the hospital within 30 days of discharge, highlighting a critical gap in care during this transition phase.
Poorly managed transitions contribute to a cascade of negative consequences:
- Increased Adverse Events: Lack of proper follow-up, medication errors, and inadequate understanding of discharge instructions can lead to preventable adverse events, compromising patient safety.
- High Readmission Rates: Readmissions are costly for both patients and the healthcare system. They disrupt patients’ lives, increase healthcare expenditures, and can indicate underlying issues in the initial care or discharge process.
- Financial Penalties for Hospitals: Healthcare systems, particularly in the US, face financial penalties from organizations like the Centers for Medicare & Medicaid Services (CMS) for high readmission rates for certain conditions. This financial pressure incentivizes hospitals to invest in effective transitional care strategies.
- Reduced Patient Satisfaction: Patients who feel unsupported or unprepared after discharge are less likely to be satisfied with their care experience overall.
- Strain on Healthcare Resources: Preventable readmissions and emergency department visits place unnecessary strain on already burdened healthcare resources.
Transitional care programs are designed to directly address these risks by proactively managing the transition process. By focusing on patient education, medication management, communication, and follow-up, these programs aim to prevent adverse events, reduce readmissions, improve patient outcomes, and enhance the overall quality and efficiency of healthcare delivery.
Key Strategies and Models in Transitional Care Programs
Effective transitional care programs often incorporate a combination of strategies categorized as predischarge, postdischarge, and bridging interventions.
Predischarge Interventions: These actions are initiated while the patient is still hospitalized and lay the groundwork for a smooth transition. Common predischarge interventions include:
- Risk Assessment: Identifying patients at high risk for readmission or adverse events allows for targeted interventions and resource allocation.
- Patient Engagement and Education: Providing clear, understandable discharge instructions, educating patients and caregivers about their condition, medications, follow-up appointments, and warning signs.
- Individualized Care Plans: Developing personalized discharge plans that address the patient’s specific needs, preferences, and resources.
- Medication Reconciliation: Reviewing and reconciling medications to ensure accuracy and address potential drug interactions.
- Communication with Outpatient Providers: Initiating communication with the patient’s primary care physician or other outpatient providers to ensure a seamless handover of care.
- Multidisciplinary Discharge Planning Teams: Involving nurses, physicians, social workers, pharmacists, and other healthcare professionals in the discharge planning process to provide comprehensive support.
Postdischarge Interventions: These strategies extend support into the post-hospital period to reinforce the discharge plan and address any emerging issues. Postdischarge interventions often include:
- Outreach to Patients: Follow-up phone calls, emails, or text messages to check on the patient’s well-being, answer questions, and reinforce discharge instructions. Some programs utilize patient-activated hotlines for easy access to support.
- Home Visits: In some cases, home visits by nurses or other healthcare professionals may be necessary to assess the patient’s environment, provide hands-on support, and monitor their condition.
- Facilitated Clinical Follow-up: Assisting patients in scheduling and attending follow-up appointments with their primary care physician or specialists.
- Postdischarge Medication Reconciliation: Re-verifying medications after discharge to address any changes or discrepancies and ensure adherence.
Bridging Interventions: The most effective transitional care programs often utilize “bridging” strategies, which combine both predischarge and postdischarge components. These integrated approaches provide continuous support throughout the transition process, maximizing their impact.
Several established and well-researched transitional care models exemplify these bridging strategies:
- Care Transitions Intervention (CTI): This model focuses on patient empowerment and self-management. A “transition coach” (often a nurse) works with patients both before and after discharge, focusing on four pillars: medication self-management, personal health record, follow-up with primary care, and recognizing “red flags.” CTI has demonstrated significant reductions in readmission rates in various patient populations.
- Transitional Care Model (TCM): Led by a transitional care nurse (TCN), TCM targets high-risk older adults with chronic illnesses. The TCN follows patients from hospital to home, providing home visits and phone follow-up, emphasizing multidisciplinary care coordination. TCM has shown significant reductions in readmissions and improved outcomes for geriatric patients.
- Project Re-Engineered Discharge (RED): Project RED is a team-based approach coordinated by a nurse discharge advocate (DA). It includes a comprehensive discharge plan, medication reconciliation, and pharmacist-led postdischarge phone follow-up. Project RED has demonstrated reductions in hospital utilization, including emergency department visits and readmissions.
- Project Better Outcomes for Older Adults Through Safe Transitions (BOOST): BOOST is a quality improvement program that provides hospitals with tools and mentorship to implement transitional care strategies. It emphasizes risk assessment, medication reconciliation, discharge checklists, and multidisciplinary teamwork. BOOST has shown modest reductions in readmission rates across various hospital settings.
Table 1. Taxonomy of Interventions to Improve Transitional Care at Hospital Discharge. Effective programs often incorporate elements from each category: predischarge, postdischarge, and bridging interventions.
Transitional Care Programs for Neurological Patients
Patients with neurological conditions, such as stroke, epilepsy, multiple sclerosis, and Parkinson’s disease, often face unique challenges during transitions of care. They may have complex medical needs, cognitive impairments, physical disabilities, and require ongoing rehabilitation and support. Transitional care programs tailored to these patients are particularly important.
While general transitional care principles apply, programs for neurological patients may incorporate specific elements:
- Stroke-Specific Interventions: For stroke patients, programs may focus on secondary stroke prevention (medication adherence for antithrombotics, antihypertensives, lipid-lowering agents), dysphagia screening and management, and early rehabilitation planning.
- Neuro-Rehabilitation Integration: Ensuring a smooth transition to outpatient rehabilitation services (physical therapy, occupational therapy, speech therapy) is crucial for neurological recovery.
- Symptom Management Protocols: Providing patients and caregivers with strategies to manage neurological symptoms such as pain, fatigue, spasticity, and bowel/bladder dysfunction.
- Home Care and Disease Monitoring: Establishing home care services for ongoing monitoring of neurological conditions and medication management.
- Direct Communication with Rehabilitation Programs: Facilitating communication between hospital-based providers and outpatient rehabilitation teams to ensure coordinated care.
Neurohospitalists, specialists in hospital-based neurological care, play a vital role in implementing and optimizing transitional care programs for neurological patients. Their expertise in neurological conditions allows them to identify specific patient needs and tailor interventions to improve outcomes and reduce readmissions in this vulnerable population.
Implementing a Successful Transitional Care Program
Implementing an effective transitional care program requires a systematic and multidisciplinary approach. Key considerations for hospitals and healthcare organizations include:
- Data Analysis: Start by analyzing your hospital’s readmission data, identifying trends, and pinpointing patient populations at highest risk. Understand your current 30-day readmission rates for all causes and for specific conditions.
- Infrastructure Assessment: Evaluate your hospital’s existing quality improvement and patient safety infrastructure. Consider the capabilities of your electronic health record (EHR) system and your organization’s prior experience with quality improvement initiatives.
- Team Building: Create an interdisciplinary team to lead the transitional care program implementation. This team should include physicians, nurses, social workers, pharmacists, care managers, administrators, and potentially patient representatives. Identify champions within each discipline to drive the initiative.
- Outcome Measurement: Define specific, measurable, achievable, relevant, and time-bound (SMART) goals for your program. Focus on key outcomes such as 30-day readmission rates, adverse drug events, emergency department visits, and patient satisfaction.
- Strategy Selection: Choose a bundled, multicomponent transitional care strategy that aligns with your hospital’s resources and patient population needs. Consider adopting or adapting established models like CTI, TCM, Project RED, or BOOST.
- Key Component Integration: Ensure your program incorporates essential elements: patient engagement, a dedicated transitions provider, medication reconciliation, facilitated communication with outpatient providers, and proactive patient outreach.
- Disease-Specific Adaptations: Incorporate disease-specific interventions as needed, particularly for high-risk populations like neurological patients.
- Implementation and Training: Develop a detailed implementation plan and provide comprehensive training to all staff involved in the transitional care process.
- Monitoring and Evaluation: Continuously monitor program performance using the defined outcome measures. Regularly evaluate the program’s effectiveness, identify areas for improvement, and make data-driven adjustments to optimize outcomes.
- Sustainability: Consider the long-term sustainability of the program, including resource allocation, staffing models, and integration into routine clinical workflows.
Table 2. Summary Recommendations for Neurohospitalists. These recommendations highlight key actions for neurohospitalists to improve transitional care for their patients, focusing on data utilization, team collaboration, and evidence-based interventions.
Conclusion: Investing in Seamless Patient Transitions
Transitional care programs are not merely a checklist of tasks; they represent a fundamental shift towards a more patient-centered and proactive approach to healthcare. By investing in well-designed and diligently implemented transitional care programs, hospitals and healthcare systems can significantly improve patient safety, reduce costly readmissions, enhance patient satisfaction, and contribute to a more efficient and effective healthcare system. Understanding “what is a transitional care program” and its critical components is the first step towards building a healthcare future where every patient experiences a safe and supported journey from hospital to home and beyond. For patients with complex conditions, particularly neurological disorders, these programs are not just beneficial—they are essential for optimizing recovery, preventing complications, and ensuring the best possible quality of life.