Hospitals today face increasing pressure to refine their transitional care practices. The goal? To lower 30-day readmission rates, prevent post-discharge adverse events, and ensure a seamless and safe transition for patients moving from hospital to home. Despite the growing recognition of the importance of transitional care, concrete evidence demonstrating significant reductions in readmission rates, especially for vulnerable populations like stroke patients, remains limited. Effective hospital-led transition care programs often incorporate a “bridging” approach, combining interventions before and after discharge, and rely on dedicated transition providers throughout the process. While implementing comprehensive strategies that include patient engagement, dedicated transition teams, and improved communication with outpatient services demands resources, studies suggest that neurohospitalists can successfully establish transitional care programs to enhance patient safety across the entire continuum of care.
Defining Transition Care Programs and Their Importance
What is a Transition Care Program?
A transition care program is designed to support patients as they move between different healthcare settings and providers. This crucial phase, often referred to as transitional care, aims to bridge gaps in care that can occur during these transitions, such as moving from inpatient hospital care to outpatient or home-based care. These programs are specifically designed to smooth the transition from a hospital stay to the outpatient environment, proactively working to prevent unnecessary hospital readmissions and post-discharge adverse events.
The period immediately following hospital discharge is a particularly vulnerable time for patients. Alarmingly, about one in five patients experience adverse events in the weeks after leaving the hospital, including adverse drug events (ADEs) and other hospital-related complications. Readmission rates are also high, with nearly 20% of older Medicare patients being readmitted to the hospital within 30 days of discharge.
A wide range of adverse events can occur post-discharge, from diagnostic errors to therapeutic errors. However, ADEs are especially prevalent and harmful, frequently leading to hospitalizations and readmissions. Recent data indicates that almost 100,000 elderly patients are hospitalized each year due to ADEs. Patients who have experienced a stroke are at an even greater risk for recurrent cerebrovascular events, repeated hospitalizations within a year of their initial admission, increased disability, and higher mortality rates. For neurohospitalists, ensuring safe care transitions for patients with complex, chronic neurological conditions such as stroke, demyelinating diseases, epilepsy, and neuromuscular disorders remains a critical patient safety priority.
The Risk of Readmissions and Adverse Events
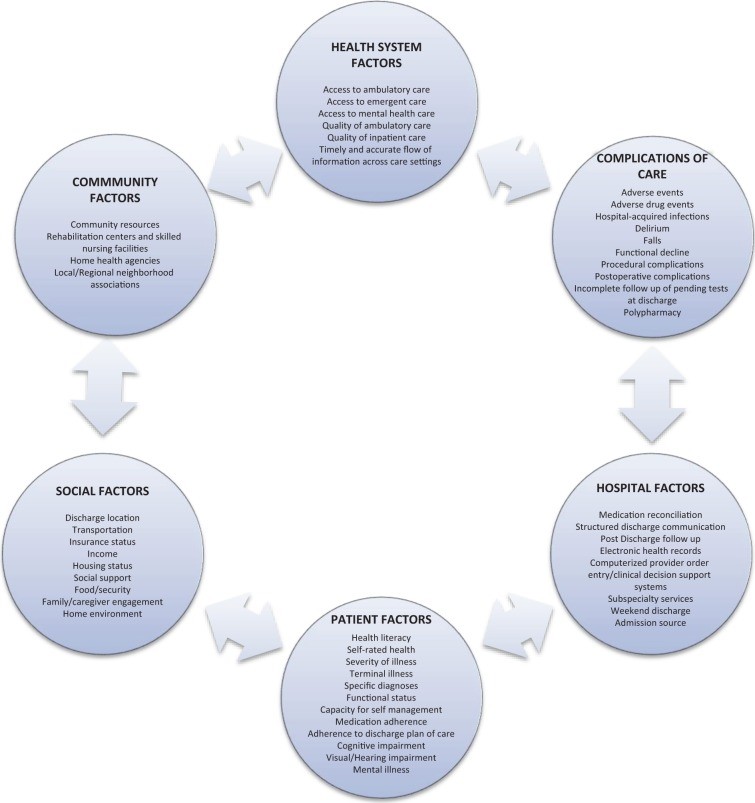
Predicting precisely which patients will be readmitted or suffer an adverse event after discharge is challenging. However, certain patient groups face a heightened risk during the post-hospitalization period. These include older adults, individuals with chronic illnesses, and those hospitalized for conditions like stroke. This increased risk is often due to fragmented care, transitions across multiple care sites, and frequent handoffs between different healthcare providers. Factors such as poor functional status at discharge, advanced age, psychiatric illness, and limited social support services have been identified as significant risk factors for hospital readmission and poorer outcomes in neurology patients. Despite these known risk factors, a systematic review evaluating predictors of readmission after stroke found a lack of reliable, standardized models for predicting readmissions across different hospitals.
Even without perfect prediction models, it’s clear that older adults and those with multiple chronic conditions constitute a significant portion of hospital admissions and readmissions within neurology services. Stroke patients, in particular, are frequently readmitted for cerebrovascular issues, cardiac conditions, and non-cardiac problems like urinary tract infections, pneumonia, and fractures. Studies suggest that a substantial percentage of 30-day readmissions – potentially as high as 20% – are preventable. These readmission rates are often influenced by factors outside the hospital environment, including inadequate social support, poverty, and limited access to outpatient care. A review of stroke and cerebrovascular disease discharges at one academic medical center revealed that over half of readmissions were potentially avoidable, citing issues like gaps in care coordination, delayed follow-up, and insufficient discharge instructions.
Key Strategies in Transition Care Programs
To address these challenges, transition care programs employ a range of strategies, broadly categorized into predischarge, postdischarge, and bridging interventions. Predischarge interventions occur while the patient is still in the hospital and include:
- Risk Assessment: Evaluating the patient’s risk of adverse events or readmission.
- Patient Engagement: Educating patients and caregivers about their condition and post-discharge care.
- Personalized Patient Records: Creating easy-to-understand discharge instructions and summaries.
- Communication with Outpatient Providers: Facilitating communication between hospital and outpatient teams.
- Multidisciplinary Discharge Planning: Involving a team of healthcare professionals in discharge planning.
- Dedicated Transition Provider: Assigning a specific person to oversee the transition process.
- Medication Reconciliation: Reviewing and reconciling medications to prevent errors.
Postdischarge interventions are implemented after the patient leaves the hospital and may include:
- Patient Outreach: Follow-up phone calls, hotlines, and home visits to check on patients.
- Facilitated Clinical Follow-up: Assisting patients in scheduling and attending follow-up appointments.
- Post-discharge Medication Reconciliation: Re-verifying medications after discharge.
Bridging interventions combine elements of both predischarge and postdischarge strategies, providing continuous support throughout the transition period. These comprehensive strategies are often the most effective in ensuring a safe and successful transition.
Examples of Effective Transition Care Programs
Several nationally recognized transition care programs have demonstrated success in reducing readmissions and improving patient outcomes. These programs offer valuable models for hospitals looking to enhance their own transition care services.
Care Transitions Intervention (CTI)
The Care Transitions Intervention (CTI), developed by Eric Coleman, is a multi-component program focused on patient empowerment and self-management. It has been implemented in various hospital settings and studied in older adults, including those with stroke and chronic illnesses. CTI focuses on four key areas: medication management, personal health record maintenance, primary care provider follow-up, and recognizing “red flags” that require contacting providers. A “transition coach,” often an advanced practice nurse, provides home visits and phone calls to reinforce patient engagement and self-management skills. Studies have shown that CTI significantly reduces 30-day readmission rates across different healthcare delivery systems.
Transitional Care Model (TCM)
The Transitional Care Model (TCM), pioneered by Mary Naylor, is a nurse-led program targeting high-risk, chronically ill older adults. While studies haven’t specifically focused on neurology patients, TCM has been effective in populations with CHF and myocardial infarction. A transitional care nurse (TCN) follows patients from the hospital to home, acting as a central point of contact and facilitating communication between inpatient and outpatient providers. TCM emphasizes a multidisciplinary approach, with the TCN collaborating with physicians, nurses, social workers, and pharmacists. Research has demonstrated significant reductions in readmission rates at 60 and 90 days with the TCM.
Project Re-Engineered Discharge (RED)
Project Re-Engineered Discharge (RED) is a team-based program emphasizing a multidisciplinary approach coordinated by a nurse discharge advocate (DA). Developed for general medicine patients in an urban safety-net hospital, RED involves the DA engaging patients during hospitalization and providing them with clear, personalized discharge plans. Post-discharge, a pharmacist conducts follow-up phone calls, including medication reviews and direct communication with the patient’s primary care provider. Project RED has shown significant reductions in hospital utilization, measured as combined emergency department visits and readmissions within 30 days of discharge.
Project Better Outcomes for Older Adults Through Safe Transitions (BOOST)
Project BOOST (Better Outcomes for Older Adults Through Safe Transitions), supported by the Society of Hospital Medicine, is a quality improvement collaborative implemented across diverse US hospitals. BOOST provides a toolkit and mentorship to hospitals to develop and implement site-specific transition care programs. Key components of BOOST include risk assessment, medication reconciliation, discharge checklists, and a multidisciplinary team approach to discharge planning. Studies have indicated that BOOST implementation can lead to modest reductions in 30-day readmission rates.
Strategies for Neurologic Patients
While general transition care programs offer valuable frameworks, specific strategies are crucial for patients with neurological conditions like stroke. A systematic review of transitional care for stroke patients suggests that hospital-initiated interventions can improve outcomes like reduced hospital stays and improved physical activity. However, evidence for reducing readmissions or mortality in this population is less conclusive in some studies. Despite this, experts emphasize the importance of care coordination for improved healthcare in stroke patients. Specific interventions like secondary stroke prevention measures (antithrombotics, antihypertensives, lipid-lowering agents), dysphagia screening, and reducing unnecessary urinary catheter use have been shown to reduce readmissions and post-discharge adverse events in this population. Neurohospitalists are uniquely positioned to implement these targeted interventions, improving care quality, reducing costs, and mitigating risks associated with preventable readmissions and adverse events for their patients.
Common Features and Implementation of Successful Programs
Common Elements of Effective Programs
Despite their variations, successful transition care programs share common features. Many programs, both general and stroke-specific, utilize bridging interventions with a dedicated transition provider, such as a nurse or case manager, as the clinical lead. A central theme is the presence of an advocate who facilitates care coordination and proactively reaches out to patients post-discharge. For both general medicine and neurology patients, strategies focused on improving communication across care settings, proactive outreach, and robust patient engagement are key to positive outcomes.
Implementation and Cost Considerations
While descriptions of transition care programs often detail interventions and timelines, information regarding implementation costs, resource needs, and sustainability efforts is often limited. Hospitals considering implementing or improving transition care programs need to carefully evaluate these factors to ensure long-term success and impact.
Recommendations for Neurohospitalists and Hospitals
Hospitals and neurohospitalists are tasked with developing effective strategies to reduce readmissions and avoid financial penalties associated with high readmission rates. Research consistently points to the effectiveness of multidisciplinary, multi-component strategies that incorporate bridging interventions and dedicated transition clinicians. Programs like CTI, TCM, Project RED, and Project BOOST offer proven models that have been successfully adapted and implemented across various healthcare settings.
It’s crucial to recognize that there is no “one-size-fits-all” approach to transition care. Each hospital network has unique internal factors, culture, community demographics, and geographic considerations that must be taken into account. However, the foundational elements of a successful transition care strategy are consistent: patient engagement, a dedicated transition provider, comprehensive medication management (including reconciliation), facilitated communication with outpatient providers, and proactive patient outreach. For neurology patients, disease-specific interventions, such as home care protocols for disease monitoring, medication adherence support, symptom management plans, and direct connections with rehabilitation programs, can further enhance program effectiveness.
Neurohospitalists are uniquely positioned to drive improvements in transition care for a broad spectrum of patients, both as primary providers and consultants. They can champion specific initiatives, such as delirium and dysphagia screening for neurology patients, or collaborate with hospitalist colleagues on institution-wide transition care strategies. As consultants, neurohospitalists can provide evidence-based recommendations to minimize readmission risks and adverse events, particularly regarding secondary stroke prevention.
To effectively enhance transition care, neurohospitalists should prioritize the following practical recommendations for all patients they admit:
- Patient Engagement: Provide thorough counseling on medication management, “red flags” for worsening conditions, disease-specific management techniques, and available resources for post-discharge support.
- Communication with Outpatient Providers: Ensure seamless communication with rehabilitation facilities, skilled nursing facilities, and outpatient physicians to facilitate appropriate follow-up, medication reconciliation, and ongoing care management.
- Outreach: Implement follow-up phone calls or home visits, when feasible, to proactively address any issues and ensure a safe and supported transition home.
By focusing on these key areas and adapting proven transition care program models, hospitals and neurohospitalists can significantly improve patient safety, reduce preventable readmissions, and enhance the overall quality of care delivered during this critical transition period.
References
References are in the original article. (Note: In a real-world scenario, the references would be copied here.)