Coordinated Care Programs are designed to streamline and enhance the healthcare experience for individuals with complex needs, often those eligible for both Medicare and Medicaid, also known as dual eligibles. These programs, like the Commonwealth Coordinated Care (CCC) in Virginia, aim to integrate primary, acute, behavioral, and long-term services to provide more holistic and efficient care. A key feature of these programs is the option for eligible individuals to enroll, but equally important is their right to decline participation. This is where the “opt-out form” comes into play.
This article delves into the concept of a coordinated care program opt-out form, drawing insights from the Virginia CCC program to provide a comprehensive understanding for beneficiaries and stakeholders alike.
Understanding Coordinated Care Programs and Enrollment
Before diving into the opt-out form, it’s crucial to understand the basics of coordinated care programs. These initiatives are often state-led, in partnership with federal programs like Medicaid and Medicare, to improve care quality and manage costs for dual eligible beneficiaries. In Virginia’s CCC program, eligible individuals are enrolled in Medicaid-Medicare Plans (MMPs) that manage their care coordination.
Enrollment into such programs can be voluntary or automatic, often referred to as “passive enrollment.” In the case of Virginia’s CCC, eligible beneficiaries initially receive information about the program and the option to voluntarily enroll. If they do not actively choose a plan, they are then notified about automatic enrollment, with continued opportunities to opt-out or select a plan.
The Significance of Choice: Opting Out
The ability to opt-out of a coordinated care program is a fundamental right for beneficiaries. It acknowledges that while these programs offer potential benefits, they may not be the best fit for everyone. Individuals might prefer to maintain their existing healthcare arrangements, providers, or simply feel that a managed care approach doesn’t align with their needs.
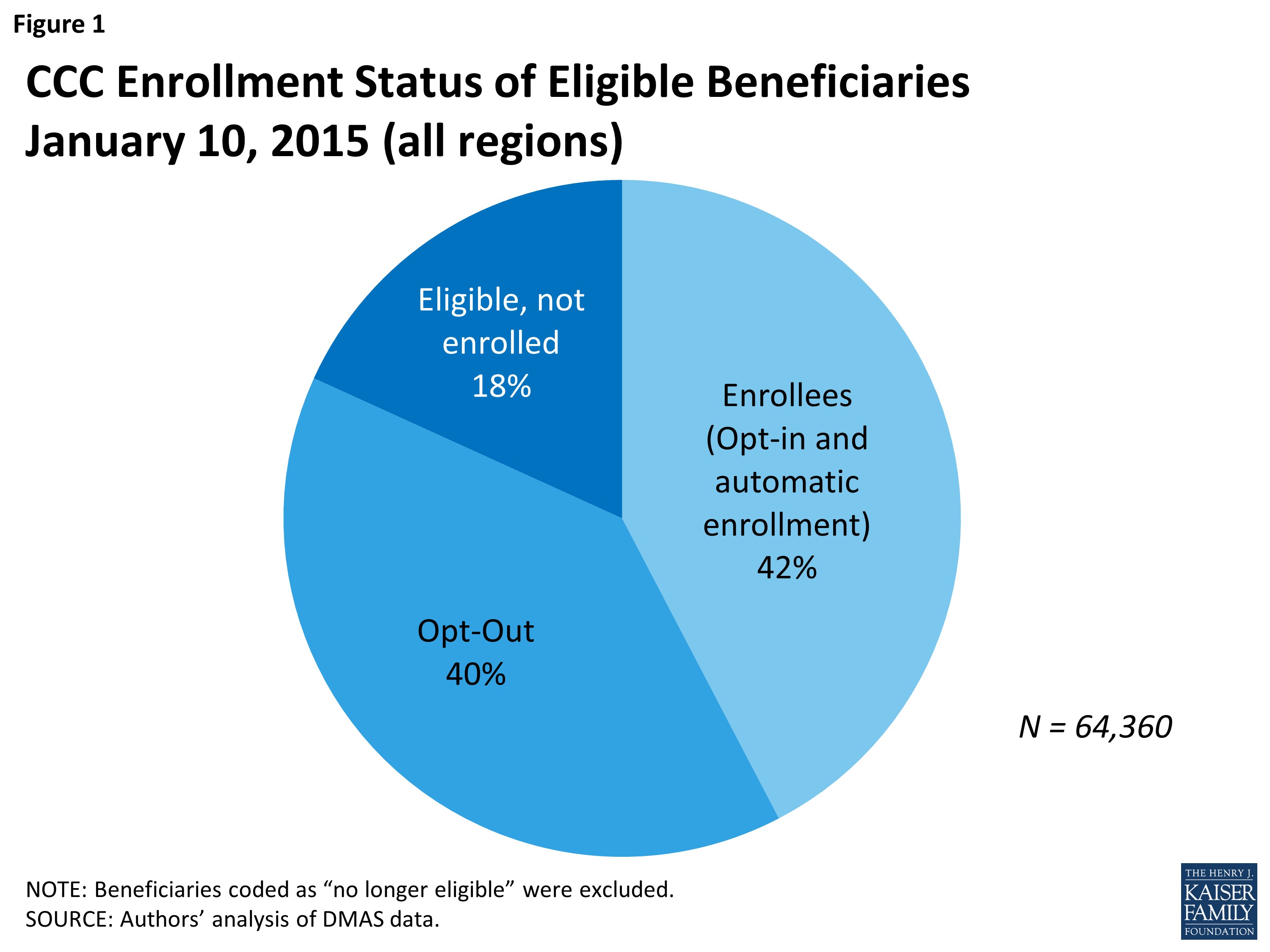
Figure 1 illustrates the enrollment status in Virginia’s CCC program, highlighting a significant percentage of eligible beneficiaries who opted out, demonstrating the relevance and utilization of the opt-out option.
What is a Coordinated Care Program Opt-Out Form?
A coordinated care program opt-out form is an official document that allows eligible individuals to formally decline enrollment or participation in a coordinated care program. This form serves as a clear and documented way for beneficiaries to exercise their right to choose not to participate in the program, even if they are eligible.
Key Purposes of the Opt-Out Form:
- Formal Declination: It provides a formal mechanism for beneficiaries to state their decision to not enroll in the coordinated care program.
- Informed Choice: The form and accompanying information are intended to ensure beneficiaries are aware of their option to opt-out, promoting informed decision-making.
- Program Management: For program administrators, the opt-out form helps track enrollment decisions, understand opt-out rates, and manage program participation effectively.
- Maintaining Current Coverage: Opting out ensures that individuals can continue with their current healthcare coverage, whether it’s traditional Medicare and Medicaid or other arrangements.
In Virginia’s CCC program, beneficiaries were informed of their right to opt-out in initial letters introducing the program. This proactive communication is essential to ensure beneficiaries are aware of their choices from the outset.
Why Might Someone Choose to Opt-Out?
Understanding the reasons why beneficiaries might opt-out is crucial for improving coordinated care programs and ensuring they truly meet the needs of their target population. Data from the Virginia CCC program reveals several key reasons for opting out:
- Satisfaction with Current Coverage: A significant majority of those who opted out in Virginia indicated they were satisfied with their existing Medicaid and Medicare coverage. This suggests that for some, the perceived benefits of the new program did not outweigh the comfort and familiarity of their current arrangements.
- Provider Network Concerns: Another major reason for opting out was the concern that current providers might not be participating in the program’s network. Continuity of care with trusted providers is a high priority for many, especially those with complex health needs.
Figure 4 highlights the regional variations in opt-out rates within the Virginia CCC program, suggesting that factors like program awareness and network adequacy can influence beneficiaries’ decisions to opt-out.
- Confusion and Lack of Understanding: The introduction of a new healthcare program can be confusing. Some beneficiaries may opt-out simply because they don’t fully understand the program, its benefits, or how it might affect their care. Clear and accessible communication is vital to address this.
- Preference for Fee-for-Service: Some individuals prefer the fee-for-service model, valuing the flexibility and choice it offers. They might be wary of managed care approaches inherent in coordinated care programs, which may have network limitations and require prior authorizations.
- Influence of Providers: As noted in the Virginia case study, some providers initially wary of the CCC program might have influenced beneficiaries’ decisions to opt-out. This underscores the importance of engaging and educating providers about the benefits of coordinated care programs.
The Opt-Out Process: Key Steps
The process for opting out of a coordinated care program should be straightforward and accessible. Based on the Virginia CCC program’s experience, here are typical steps involved in the opt-out process:
- Notification and Information: Eligible beneficiaries are informed about the coordinated care program, its benefits, and their right to opt-out. This is often done through letters and informational materials.
- Opt-Out Form Availability: An opt-out form is made readily available to beneficiaries. This form might be included in the initial information packet, available online, or accessible through enrollment brokers or program helplines.
- Submission of the Form: Beneficiaries who decide to opt-out need to complete and submit the form through specified channels. This could be via mail, fax, or online portal.
- Confirmation of Opt-Out: After processing the opt-out form, program administrators should provide confirmation to the beneficiary, acknowledging their decision and clarifying their coverage status.
- Ongoing Opt-Out Option: Beneficiaries usually retain the right to opt-out at any time, not just during the initial enrollment period. This flexibility ensures that individuals can make choices that best suit their evolving needs.
In Virginia, beneficiaries were given multiple opportunities to opt-out throughout the enrollment process, demonstrating a commitment to beneficiary choice and control.
Implications of Opting Out
Opting out of a coordinated care program means that beneficiaries will not receive care coordination and enhanced benefits offered by the program’s MMPs. They will revert to or continue with their existing healthcare coverage, typically traditional fee-for-service Medicare and Medicaid.
Key implications to consider:
- Loss of Enhanced Benefits: Beneficiaries will forgo any extra benefits offered by the coordinated care program, such as additional dental, vision, or transportation services.
- Traditional Care Coordination: They will rely on the standard care coordination mechanisms within the traditional Medicare and Medicaid systems, which may be less integrated compared to the coordinated care program.
- Continuity of Existing Coverage: Opting out ensures uninterrupted continuation of their current healthcare coverage and provider relationships, which is a significant advantage for those satisfied with their current care.
Conclusion: Empowering Beneficiaries Through Choice
The coordinated care program opt-out form is more than just a procedural document; it is a symbol of beneficiary rights and informed choice within evolving healthcare systems. It ensures that while coordinated care programs aim to improve healthcare delivery, participation remains a choice, respecting individual preferences and circumstances.
Understanding the “what, why, and how” of opt-out forms is essential for beneficiaries, advocates, and program administrators. By ensuring clear communication, accessible processes, and responsiveness to beneficiary concerns, coordinated care programs can better serve their intended populations and achieve their goals of improved health outcomes and efficient care delivery. The experience of Virginia’s CCC program provides valuable lessons for other states implementing similar initiatives, highlighting the importance of balancing program goals with the fundamental right of beneficiaries to make informed choices about their healthcare.