Hospital readmissions and post-discharge adverse events are significant challenges in healthcare systems worldwide. A particularly vulnerable period for patients is immediately following their discharge from a hospital. During this time, many individuals experience adverse drug events, hospital-related complications, and other issues that can lead to readmission. To combat these problems and ensure patient safety as individuals move from hospital to home or other care settings, healthcare providers and policymakers are increasingly focusing on transition care programs. But What Is A Transition Care Program, and why are they so vital?
This article delves into the concept of transition care programs, exploring their definition, importance, key components, and effectiveness. We will examine successful models and strategies, particularly within the context of neurological conditions like stroke, and offer recommendations for healthcare professionals looking to implement or enhance these crucial programs.
Defining Transition Care Programs and Their Importance
To understand what is a transition care program, we first need to define transitional care itself. Transitional care refers to the coordinated set of actions designed to ensure the safe and seamless transfer of patients between different healthcare settings and providers. This includes moving patients from hospitals to their homes, rehabilitation facilities, skilled nursing facilities, or even between different units within a hospital. A transition care program is then a structured, organized approach to delivering this transitional care. It’s a specific set of interventions and strategies implemented to bridge gaps in care during these transitions.
What is Transitional Care?
At its core, transitional care aims to prevent disruptions in patient care as they move across the healthcare continuum. It recognizes that these transition points are often vulnerable times where communication breakdowns, medication errors, lack of follow-up, and inadequate patient education can occur, leading to negative health outcomes.
Imagine a patient recovering from a stroke in a hospital. Their care team in the hospital is well-coordinated, managing their medications, therapy, and monitoring their condition closely. However, upon discharge, the patient and their family become responsible for managing medications, attending follow-up appointments, and recognizing potential complications at home. Without a structured transition care program, this shift in care responsibility can be overwhelming and risky.
Why are Transition Care Programs Important?
The importance of transition care programs stems from several critical factors:
- Reducing Hospital Readmissions: A significant driver for the focus on transitional care is the high rate of hospital readmissions. In many countries, a substantial percentage of older adults are readmitted to hospitals within 30 days of discharge. These readmissions are costly and often preventable. Transition care programs are designed to directly address the factors contributing to preventable readmissions.
- Preventing Adverse Events: The period after hospital discharge is associated with a high risk of adverse events, particularly adverse drug events (ADEs). These events can result from medication errors, lack of understanding of discharge instructions, or inadequate follow-up. Transition care programs implement strategies to minimize these risks.
- Improving Patient Safety and Quality of Care: Ultimately, transition care programs are about enhancing patient safety and the overall quality of healthcare. By ensuring smooth transitions, these programs contribute to better patient outcomes, improved patient satisfaction, and a more coordinated healthcare experience.
- Responding to Policy Initiatives: Government healthcare agencies, like the Centers for Medicare & Medicaid Services (CMS) in the United States, are increasingly focused on hospital readmission rates. Financial penalties are often imposed on hospitals with high readmission rates, further incentivizing the implementation of effective transition care programs. These policies recognize that improving transitional care is a key opportunity to reduce healthcare expenditures and improve population health.
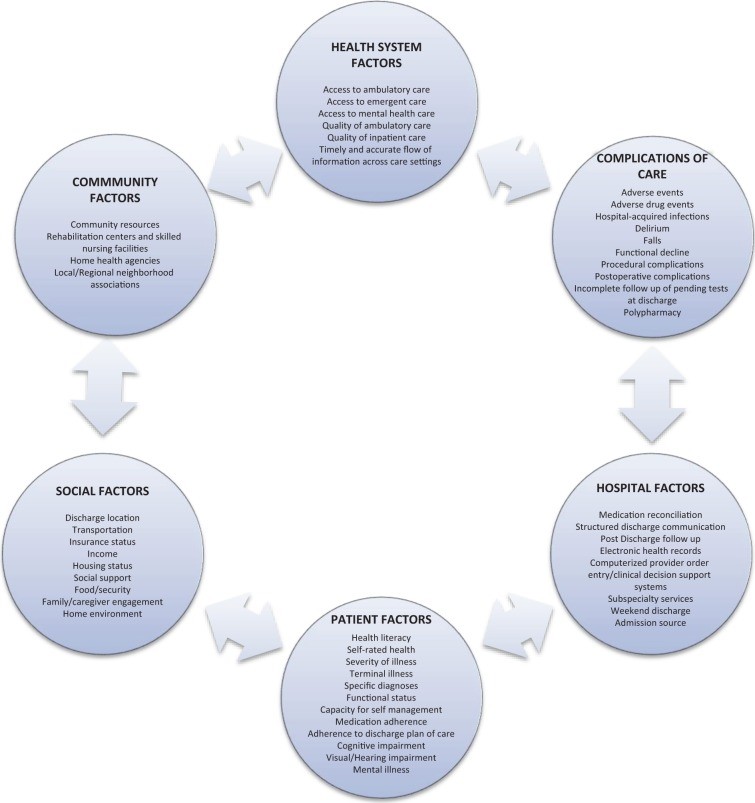 Figure 1.
Figure 1.
Alt text: Diagram illustrating factors contributing to hospital readmission, categorized into hospital domain, patient characteristics, and external factors such as poor social support and access to outpatient care.
Key Components of Effective Transition Care Programs
While the specifics of transition care programs can vary, successful models often share common key components. These elements work together to create a comprehensive approach to supporting patients during care transitions.
Bridging Strategies
Effective transition care programs typically employ “bridging” strategies. This means they include interventions that occur both before and after hospital discharge. This dual approach ensures continuity of care and support throughout the entire transition period. Predischarge interventions prepare the patient and their caregivers for the transition, while post-discharge interventions provide ongoing support and address any emerging issues after the patient is home.
Dedicated Transition Provider
A cornerstone of many successful programs is the involvement of a dedicated transition provider. This could be a nurse, case manager, pharmacist, or social worker specifically trained in transitional care. This provider serves as a consistent point of contact for the patient, coordinating care, providing education, and facilitating communication between different healthcare providers. Having a dedicated individual responsible for overseeing the transition significantly improves coordination and reduces the chances of patients getting lost in the system.
Patient Engagement
Engaging patients and their caregivers is paramount. Transition care programs emphasize patient education, self-management skills, and shared decision-making. Patients need to understand their medications, follow-up appointments, potential red flags to watch out for, and how to access support if needed. Providing patients with personalized health records, clear discharge instructions in lay language, and opportunities to ask questions are crucial elements of patient engagement.
Medication Management and Reconciliation
Medication errors are a leading cause of post-discharge adverse events and readmissions. Transition care programs incorporate robust medication management strategies, including medication reconciliation. This involves carefully reviewing all of a patient’s medications – both before and during hospitalization – and creating an accurate medication list at discharge. Patients and caregivers receive clear instructions on how to take their medications, potential side effects, and when to seek help. Post-discharge medication reconciliation, often through follow-up phone calls, further ensures medication safety.
Communication with Outpatient Providers
Seamless communication between hospital-based providers and outpatient providers is essential. Transition care programs facilitate this communication by ensuring that primary care physicians and specialists receive timely and comprehensive discharge summaries. This information should include the patient’s diagnosis, treatment during hospitalization, medication list, follow-up needs, and any outstanding issues. Direct communication, such as phone calls or secure messaging, can further enhance care coordination.
Patient Outreach
Post-discharge outreach is a proactive strategy to identify and address potential problems early. This often involves follow-up phone calls by a transition provider within a few days of discharge. These calls can assess the patient’s condition, answer questions, reinforce discharge instructions, and ensure they are attending follow-up appointments. In some cases, home visits may be part of the outreach strategy, particularly for high-risk patients. Patient-activated hotlines also provide a readily accessible resource for patients to seek help or advice after discharge.
Examples of Successful Transition Care Programs
Several well-established transition care programs have demonstrated effectiveness in reducing readmissions and improving patient outcomes. These programs often serve as models for hospitals and healthcare systems looking to implement their own initiatives. Here are a few prominent examples:
Care Transitions Intervention (CTI)
Developed by Dr. Eric Coleman, the Care Transitions Intervention (CTI) focuses on empowering patients to become active participants in their post-discharge care. CTI utilizes a “transition coach,” often an advanced practice nurse, who works with patients and caregivers using four key pillars: medication self-management, creating a personal health record, ensuring follow-up appointments, and recognizing “red flags” that require contacting a provider. CTI has been shown to significantly reduce 30-day readmission rates across various healthcare settings.
Transitional Care Model (TCM)
The Transitional Care Model (TCM), pioneered by Dr. Mary Naylor, is a nurse-led program targeting chronically ill, high-risk older adults. A transitional care nurse (TCN) follows patients from the hospital to home, providing intensive support through home visits and phone calls. TCM emphasizes a multidisciplinary approach, with the TCN coordinating with physicians, nurses, social workers, and pharmacists. Studies of TCM have demonstrated significant reductions in readmission rates, particularly at 90 days post-discharge.
Project Re-Engineered Discharge (RED)
Project RED focuses on a team-based approach to discharge planning, coordinated by a nurse discharge advocate (DA). The DA educates patients, provides a personalized post-hospitalization plan, and ensures they understand their medications and follow-up care. A key component of Project RED is pharmacist-led post-discharge phone calls for medication review and communication with primary care providers. Project RED has been shown to reduce hospital utilization, including both readmissions and emergency department visits.
Project Better Outcomes for Older Adults Through Safe Transitions (BOOST)
Project BOOST, supported by the Society of Hospital Medicine, is a quality improvement collaborative that provides hospitals with a toolkit and mentorship to implement transition care programs. BOOST emphasizes risk assessment, medication reconciliation, discharge checklists, and a multidisciplinary team approach. It is designed to be adaptable to different hospital settings and has demonstrated modest reductions in readmission rates in participating hospitals.
Transition Care for Neurological Patients
Patients with neurological conditions, such as stroke, epilepsy, and multiple sclerosis, often face unique challenges during care transitions. They may have complex medication regimens, physical disabilities, cognitive impairments, and require ongoing rehabilitation and specialized care. Therefore, transition care programs for neurological patients need to be tailored to address these specific needs.
Specific Challenges for Neurological Patients
- High Risk of Recurrent Events: Patients with stroke are at increased risk of recurrent strokes and other cerebrovascular events after discharge.
- Complex Chronic Conditions: Neurological conditions are often chronic and require long-term management, making care transitions more complex.
- Functional and Cognitive Impairments: Neurological conditions can lead to physical disabilities and cognitive deficits, impacting a patient’s ability to manage their care at home.
- Need for Rehabilitation: Many neurological patients require ongoing rehabilitation services, and ensuring a smooth transition to rehabilitation programs is crucial.
Strategies for Neurological Patients
Transition care programs for neurological patients should incorporate specific strategies, including:
- Secondary Stroke Prevention: Focus on patient education and medication adherence for secondary stroke prevention measures (antiplatelet agents, antihypertensives, lipid-lowering medications).
- Dysphagia Screening and Management: Ensure patients with dysphagia (swallowing difficulties) receive appropriate dietary modifications and follow-up with speech therapy.
- Home Care and Disease Monitoring Protocols: Establish protocols for home healthcare to monitor disease progression, medication adherence, and symptom management.
- Direct Communication with Rehabilitation Programs: Facilitate direct communication and coordination between hospital teams and rehabilitation facilities or home-based rehabilitation services.
Implementation and Considerations
Implementing effective transition care programs requires careful planning and consideration of various factors.
Cost and Resources
Transition care programs require resources, including personnel (transition providers), technology (communication systems, patient education materials), and time. While the initial investment can be significant, the long-term benefits of reduced readmissions and improved patient outcomes can lead to cost savings and improved financial performance for hospitals.
Sustainability
Sustainability is crucial for the long-term success of transition care programs. Programs should be integrated into the hospital’s workflow and culture, with ongoing support from hospital leadership. Demonstrating the value and return on investment of these programs is essential for securing continued funding and resources.
Recommendations for Healthcare Professionals
For neurohospitalists and other healthcare professionals aiming to improve transitional care, several key recommendations emerge:
- Data Collection and Infrastructure: Collect data on 30-day readmission rates and adverse events to identify areas for improvement and track the impact of transition care programs. Utilize electronic health records and quality improvement infrastructure to support program implementation.
- Interdisciplinary Team: Create an interdisciplinary team to design and implement transition care programs. This team should include physicians, nurses, pharmacists, social workers, case managers, and potentially rehabilitation specialists.
- Outcome Measurement: Define clear, measurable outcomes to evaluate the effectiveness of transition care programs. Track readmission rates, adverse drug events, patient satisfaction, and other relevant metrics.
- Bundled Strategies: Implement bundled, multicomponent transition care programs that incorporate patient engagement, dedicated transition providers, medication reconciliation, communication facilitation, and patient outreach.
- Disease-Specific Interventions: Incorporate disease-specific interventions, particularly for high-risk populations like neurological patients, to address their unique needs.
Conclusion
Transition care programs are essential for ensuring patient safety, reducing hospital readmissions, and improving the quality of healthcare. By understanding what is a transition care program and implementing evidence-based strategies, healthcare professionals can significantly improve the transition experience for patients as they move between care settings. For neurological patients and other vulnerable populations, tailored transition care programs are particularly critical to address their complex needs and promote optimal health outcomes after hospital discharge. As healthcare systems continue to focus on value-based care and patient-centered approaches, transition care programs will remain a cornerstone of high-quality, coordinated healthcare delivery.