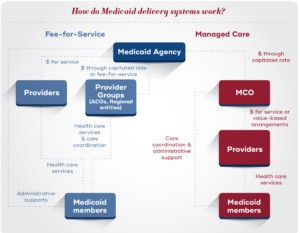
Medicaid, a cornerstone of the U.S. healthcare system, provides health coverage to nearly 90 million individuals. Far from being solely a safety net, Medicaid supports diverse populations, including low-income families, children with complex health needs, pregnant individuals, seniors, and people with disabilities. To deliver these crucial healthcare services, Medicaid agencies employ various “delivery systems,” primarily fee-for-service and managed care. Currently, managed care is the dominant model, with approximately 72% of Medicaid enrollees in comprehensive managed care plans as of 2021. This raises a critical question: is a managed care program good for Medicaid beneficiaries and the healthcare system as a whole? Let’s delve into the complexities of Medicaid managed care to understand its potential benefits and drawbacks.
Under managed care, states contract with Managed Care Organizations (MCOs) to administer Medicaid benefits. The state pays the MCO a fixed monthly rate per member, and the MCO, in turn, manages provider networks, pays for services, and coordinates care. This capitated system is designed to provide budget predictability for states and potentially improve care coordination for beneficiaries. However, the effectiveness and overall “goodness” of managed care programs are subjects of ongoing debate and research.
The Growth of Managed Care in Medicaid: A Historical Perspective
Managed care’s prominence in Medicaid is not a recent phenomenon. While prepaid health plans existed in the early 20th century, the modern managed care era was significantly influenced by the Health Maintenance Organization Act of 1973. This act encouraged the development of HMOs as an alternative to traditional fee-for-service models. Key legislative changes, such as the elimination of the “50/50” rule in 1997, further paved the way for the expansion of Medicaid managed care.
Over time, federal regulations evolved to guide the operation of Medicaid managed care plans. Section 1932 of the Social Security Act established essential safeguards concerning coverage choice, enrollment processes, member protections, and provider networks. It also mandated state oversight activities, including quality assessment and external quality reviews. These federal mandates, coupled with state-level interests in budget control and care coordination, propelled the widespread adoption of managed care models across the nation. But has this growth translated into better care and outcomes, making managed care programs genuinely “good”?
Why States Choose Managed Care: Weighing the Advantages
States often opt for managed care for several compelling reasons. Budget predictability is a major driver. Capitated payments to MCOs provide states with a fixed expenditure per member, making it easier to forecast and manage Medicaid budgets. Managed care is also perceived as offering enhanced federal flexibilities, allowing states to tailor programs to specific populations or needs. Furthermore, proponents argue that MCOs are better positioned to improve care coordination, streamline service delivery, and promote preventive care.
However, the crucial question of whether managed care genuinely improves access and quality remains complex. Academic research on managed care outcomes presents a mixed picture. Some studies suggest improvements in certain quality metrics and access to care under managed care, while others find no significant impact or even worse outcomes compared to fee-for-service. The perceived benefits of managed care, therefore, are not universally realized, and its effectiveness is highly context-dependent.
Potential Downsides and Concerns: Is Managed Care Always the Best Approach?
Despite the potential advantages, concerns exist regarding the “goodness” of managed care programs. One major concern revolves around the financial incentives of MCOs. As risk-bearing entities, MCOs are incentivized to manage costs, which could potentially lead to underutilization of necessary services. While MCOs are contracted to provide comprehensive care, the profit motive inherent in managed care raises questions about whether cost-saving measures might sometimes compromise patient care.
The debate also persists regarding care coordination. While managed care is often touted for its care coordination capabilities, some argue that provider-led entities like Accountable Care Organizations (ACOs) may be more effective in this role. ACOs, directly involved in patient care, might have a deeper understanding of patient needs and provider dynamics compared to large MCOs.
Furthermore, oversight of managed care organizations is critical. Ensuring that MCOs adhere to contract requirements, prioritize quality, and provide adequate access requires robust state oversight mechanisms. Weak oversight can lead to issues with network adequacy, service denials, and inadequate care for vulnerable populations. The “goodness” of a managed care program, therefore, heavily relies on effective regulation and monitoring.
Key Operational Components: Making Managed Care Work Effectively
To maximize the potential benefits and mitigate the risks of managed care, effective operational components are essential. These include procurement, rate setting, and oversight:
Procurement: Selecting the Right MCO Partners
The procurement process, where states select MCOs through competitive bidding, is crucial. Given the significant financial stakes and the impact on millions of lives, states must have rigorous processes to ensure they contract with high-performing MCOs. Requests for Proposals (RFPs) should clearly outline state goals, quality expectations, and member needs. A thorough evaluation process, considering factors like past performance, quality initiatives, and proposed care models, is vital for selecting MCOs that align with state objectives and can deliver “good” care.
Rate Setting: Balancing Actuarial Soundness and Service Needs
Capitation rate setting is another critical operational aspect. States must develop actuarially sound rates that adequately compensate MCOs for providing contracted services while ensuring responsible use of taxpayer dollars. This process is complex, requiring careful consideration of population health needs, service costs, and administrative expenses. Mechanisms like medical loss ratios and risk corridors can help manage financial risk and incentivize efficient and quality-focused care delivery.
Oversight: Ensuring Accountability and Quality
Robust oversight is paramount to ensuring MCO accountability and program integrity. States must actively monitor MCO performance against contract requirements, access standards, and quality metrics. This includes analyzing data on provider networks, appointment wait times, member grievances, and service utilization. Enforcement mechanisms, ranging from corrective action plans to financial penalties, are necessary to address non-compliance and ensure MCOs prioritize member well-being and quality care. Effective oversight is a cornerstone of a “good” managed care program.
The Evolving Landscape of Medicaid Managed Care
Medicaid managed care continues to evolve, reflecting changing healthcare priorities and market dynamics. States are increasingly exploring innovative approaches, such as carving out specific services or tailoring plans to specialized populations. The growth of managed Long-Term Services and Supports (MLTSS) is particularly notable, reflecting the increasing focus on integrated care for individuals with complex needs. Furthermore, there is a growing emphasis on addressing health-related social needs and reducing health disparities within managed care programs.
Market consolidation in the managed care industry is another significant trend. The increasing dominance of a few large MCOs raises questions about market competition, pricing, and potential impacts on quality and access. Regulatory changes at the federal level, such as the proposed 2023 Medicaid managed care rule, also signal a continued focus on enhancing access, quality, and financial accountability within managed care. These evolving trends will shape the future “goodness” and effectiveness of managed care programs.
Conclusion: Is Managed Care Program Good? A Nuanced Perspective
So, is a managed care program good? The answer is not a simple yes or no. Medicaid managed care presents both opportunities and challenges. It offers states budget predictability and the potential for improved care coordination. However, concerns exist regarding MCO incentives, oversight challenges, and the mixed evidence on quality and access outcomes.
Ultimately, the “goodness” of a managed care program depends heavily on its design, implementation, and ongoing oversight. States must prioritize quality, access, and member needs when contracting with and regulating MCOs. Effective procurement, actuarially sound rate setting, and robust oversight are essential for maximizing the benefits of managed care and mitigating its potential drawbacks. As Medicaid managed care continues to evolve, ongoing evaluation, innovation, and a commitment to beneficiary well-being are crucial to ensuring that these programs truly serve their intended purpose of providing high-quality, accessible healthcare to millions of Americans.
This resource was developed with support from The Commonwealth Fund, a national, private foundation based in New York City that supports independent research on health care issues and makes grants to improve health care practice and policy. The views presented here are those of the author and not necessarily those of The Commonwealth Fund, its directors, officers, or staff.