Introduction
The escalating costs of healthcare, particularly for the growing population with multiple chronic conditions, are a significant concern for healthcare systems globally. In the United States, the Centers for Medicare & Medicaid Services (CMS) recognized this challenge and, in 2015, introduced the Chronic Care Management (CCM) program. This initiative aimed to provide crucial support for Medicare beneficiaries managing two or more chronic conditions, offering a proactive approach to care outside of traditional office visits. While the clinical benefits of CCM, such as improved patient care and outcomes, are increasingly recognized, the economic advantages are equally compelling. Recent studies and articles are demonstrating how chronic care management programs save money, not only for healthcare systems but also potentially for patients themselves through reduced healthcare utilization and improved health.
A landmark study commissioned by CMS itself evaluated the initial 18 months of the CCM program and revealed striking results. Compared to a control group, patients enrolled in CCM exhibited higher rates of advance care planning and increased engagement with primary care, alongside greater utilization of home health services when needed. Crucially, the study highlighted a significant reduction in hospitalizations and emergency department visits within the CCM cohort. After accounting for the cost of the CCM program itself, the findings indicated that CCM participation led to net savings for Medicare, estimated at over $95 per patient per month, translating to tens of millions of dollars in overall savings. These findings underscored the potential of CCM not just to enhance patient care, but also to contribute significantly to healthcare cost containment.
Despite this compelling evidence and positive feedback from both patients and providers, chronic care management programs remain underutilized. This gap between potential and practice highlights the need for further exploration and dissemination of effective CCM models. To address this, a technology-driven and clinically integrated platform was developed to facilitate the scalable and evidence-based implementation of the Medicare CCM program. This platform aimed to systematically incorporate proven care management strategies and assessments into the CCM workflow, with a specific focus on identifying and mitigating patient risks. This article delves into the outcomes associated with the deployment of this platform, shedding further light on how structured chronic care management programs save money and improve patient outcomes.
Table 1. Centers for Medicare & Medicaid Services Chronic Care Management Service Elements
| Service element | Description |
|---|---|
| Initiating Visit | Initiation during an AWV, IPPE, or face-to-face E/M visit (Level 4 or 5 visit not required), for new patients or patients not seen within 1 year prior to the commencement of CCM services. |
| Structured Recording of Patient Information Using Certified Electronic Health Record (EHR) Technology | Structured recording of demographics, problems, medications, and medication allergies using certified EHR technology. A full list of problems, medications, and medication allergies in the EHR must inform the care plan, care coordination, and ongoing clinical care. |
| 24/7 Access & Continuity of Care | Provide 24/7 access to physicians or other qualified health care professionals or clinical staff including providing patients/caregivers with a means to make contact with health care professionals in the practice to address urgent needs regardless of the time of day or day of week. Continuity of care with a designated member of the care team with whom the patient is able to schedule successive routine appointments. |
| Comprehensive Care Management | Care management for chronic conditions including systematic assessment of the patient’s medical, functional, and psychosocial needs; system-based approaches to ensure timely receipt of all recommended preventive care services; medication reconciliation with review of adherence and potential interactions; and oversight of patient self-management of medications. |
| Comprehensive Care Plan | Creation, revision, and/or monitoring (as per code descriptors) of an electronic person-centered care plan based on a physical, mental, cognitive, psychosocial, functional, an environmental (re)assessment and an inventory of resources and supports; a comprehensive care plan for all health issues with a particular focus on the chronic conditions being managed. Must at least electronically capture care plan information, and make this information available timely within and outside the billing practice as appropriate. Share care plan information electronically (can include fax) and timely within and outside the billing practice to individuals involved in the patient’s care. A copy of the plan of care must be given to the patient and/or caregiver. |
| Management of Care Transitions | Management of care transitions between and among health care providers and settings, including referrals to other clinicians; follow-up after an emergency department visit; and follow-up after discharges from hospitals, skilled nursing facilities, or other health care facilities Create and exchange/transmit continuity of care document(s) timely with other practitioners and providers. |
| Home- and Community-Based Care Coordination | Coordination with home- and community-based clinical service providers. Communication to and from home and community-based providers regarding the patient’s psychosocial needs, and functional deficits must be documented in the patient’s medical record. |
| Enhanced Communication Opportunities | Enhanced opportunities for the patient and any caregiver to communicate with the practitioner regarding the patient’s care through not only telephone access, but also through the use of secure messaging, Internet, or other asynchronous non–face-to-face consultation methods. |
| Patient Consent | Inform the patient of the availability of CCM services; that only one practitioner can furnish and be paid for these services during a calendar month, and of their right to stop the CCM services at any time (effective at the end of the calendar month). Document in the patient’s medical record that the required information was explained and whether the patient accepted or declined the services. |
| Medical Decision Making | Complex CCM services require and include medical decision making of moderate to high complexity (by the physician or other billing practitioner). |

AWV, annual wellness visit; CCM, chronic care management; E/M, evaluation and management; EHR, electronic health record; IPPE, initial preventive physical examination.
The central objective of this endeavor was to develop a scalable technology and integrated clinical staff platform to effectively implement the Medicare CCM program and, crucially, to investigate the factors influencing hospitalization rates within this managed population. Understanding these factors is paramount to further optimize CCM programs and maximize their impact on both patient health and healthcare expenditure.
Methods: Building an Evidence-Based CCM Technology Platform
To ensure the CCM program was grounded in best practices and effectively addressed patient needs, a technology platform was designed incorporating evidence-based assessments and workflows. This systematic approach began with a thorough review of existing care management literature, guidelines, and protocols relevant to “in-between visit” care management. The selection of specific assessments and workflow modules for the technology platform was guided by several key criteria:
- Evidence of Utility: Prioritization was given to assessments proven effective in Medicare-age populations, ensuring relevance and impact for the target demographic of CCM programs.
- Support for Non-Face-to-Face Care: Given the nature of the CMS CCM program, assessments and tools needed to be suitable for remote delivery, facilitating efficient and effective care management outside of traditional office visits, a key element in how chronic care management programs save money by leveraging virtual care.
- Discrete Data Capture: Preference was given to assessment tools capable of generating discrete data, enabling systematic data collection, analysis, and reporting for continuous program improvement and outcome measurement.
- Risk Identification and Triggering: The platform was designed to utilize assessment results to automatically flag potential patient risks, such as falls or hospitalization, allowing for timely intervention and proactive care management.
- Actionable Insights for Improved Outcomes and Cost Reduction: The chosen assessments were intended to trigger specific actions aimed at better aligning care goals, enhancing care quality, and, importantly, reducing avoidable acute care utilization – a direct mechanism by which chronic care management programs save money for healthcare systems.
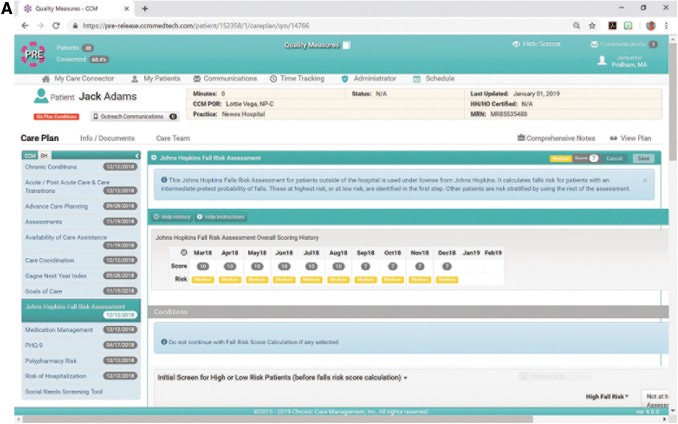
Based on these rigorous criteria, fourteen core care management modules were integrated into the CCM technology platform (Figure 1a). These modules encompassed assessments for a range of critical patient risks, including mortality, hospitalization, falls, depression, goals of care, functional status, medication management, polypharmacy, and unmet social needs. Each of these areas directly impacts patient well-being and healthcare costs, making their systematic management within the CCM framework essential for both clinical and economic success.
FIG. 1.
Depiction of the Chronic Care Management, Inc. technology platform used to support evidence-based care management workflow and patient engagement. (A) Assessments integrated into a technology platform supporting “in-between visit” chronic care management.
(B) Patient engagement methodology, showing ANNA Your Virtual Care Assistant.
Supporting Medical Groups and Clinical Staff Model
To facilitate the practical implementation of the CCM program, medical groups partnered with CCMI, leveraging CCMI’s technology and clinical staff to support their patient populations. The medical groups were responsible for identifying eligible patients, obtaining informed consent for CCM enrollment, and notifying CCMI of each enrolled patient. Critically, the patients continued to receive their regular medical care from their primary care providers within their existing care settings, ensuring continuity of care while benefiting from the added support of the CCM program.
The CCM program’s non-face-to-face support was delivered by CCMI’s clinical staff, adhering to the CMS program’s “incident-to” and general supervision requirements. This workforce consisted of licensed nurses and medical assistants who served as chronic care coordinators. Each coordinator managed an average of 400 patients, allowing for personalized attention and proactive engagement. Coordinators were organized into teams of 6-8, each overseen by an experienced licensed nurse team leader. These nurse leaders provided essential education, scheduling support, quality assurance, and served as the primary communication link between the CCM team and the participating medical practices, ensuring seamless integration and effective information flow.
Data Sources and Patient Engagement
Chronic care coordinators utilized multiple data sources to comprehensively assess patients and deliver effective CCM services. Access to the medical group’s electronic health record (EHR) was paramount, providing essential clinical information such as diagnoses, medications, visit notes, and medical histories. In cases where patients resided in assisted living or long-term care nursing facilities, nursing notes were also incorporated into the CCM data review, enriching the understanding of the patient’s overall health status. Furthermore, patient engagement data, gathered through direct patient interaction, was integrated as a valuable data source to personalize care plans and address individual needs.
Patient engagement was a cornerstone of the CCM model. Monthly outreach efforts were made to patients capable of participating in care management. For patients with SMS-enabled mobile numbers, outreach was initiated through ANNA, a virtual care assistant technology developed by CCMI. ANNA facilitated secure communication and delivered questionnaires via text message (Figure 1b). Patients without SMS capability but able to engage were contacted by coordinators via telephone. For patients with physical, mental, or cognitive limitations, coordinators communicated with their nurses or caregivers. Regardless of the outreach method, the core set of care management questions (Figure 1b) remained consistent, ensuring standardized data collection and comprehensive patient assessment across all engagement modalities.
Practitioner Engagement and Statistical Analysis
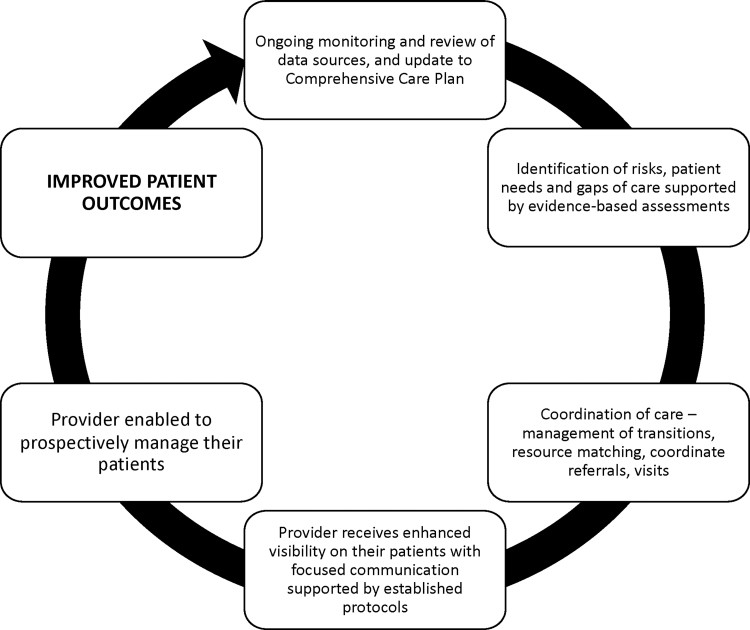
Effective practitioner engagement was crucial for the success of the CCM program. Initial implementation meetings were conducted with participating practitioners to establish clear protocols for CCM data handling, triage procedures, and preferred communication methods. When a CCM episode identified a patient risk, this information was promptly communicated to the medical practice based on the pre-defined triage protocol. Practitioners had access to review their patients’ CCM care plans and could leverage this information to refer patients to relevant resources and interventions to mitigate identified risks (Figure 2). This collaborative approach ensured that the CCM program was seamlessly integrated into the patient’s overall care plan, maximizing its effectiveness.
FIG. 2.
Practice engagement methodology.
To identify key predictors of hospitalization within the CCM patient population, binary logistic regression analysis was performed using SPSS 24.0 statistical software. The analysis considered three groups of predictor variables: (1) patient demographics (age, sex, ambulatory status, nursing home residence), (2) care planning and CCM engagement (advance care plan presence, number of CCM episodes), and (3) assessed risks (hospitalization risk, number of chronic conditions, polypharmacy risk, falls risk, and mortality risk). Mortality risk was calculated using the Gagne mortality index for community-dwelling patients and the Flacker mortality index for nursing home residents, both validated tools for predicting mortality in these populations.
Logistic regression was chosen due to the distribution of hospitalization data, with the majority of patients experiencing either zero or one hospitalization during the study period. A backward elimination procedure was employed to refine the model and identify the most significant predictors. To ensure the robustness of the model, the data was split into training and testing samples, and outlier analysis was performed to remove any undue influence from extreme data points. Receiver operating characteristic (ROC) curves were used to further evaluate the predictive power of the most influential predictors in discriminating between patients who were hospitalized and those who were not. This rigorous statistical approach provided valuable insights into the factors driving hospitalization risk within the CCM program and how chronic care management programs save money by targeting these risks.
Results: Impact and Predictors of Hospitalization in a Large CCM Cohort
Between January 1 and December 31, 2018, CCMI’s platform supported 26,500 patients under the described CCM model (Table 2). The vast majority of these patients (95.6%) resided in community settings such as private homes or senior living facilities, with a smaller proportion (4.4%) in nursing homes. The average age of the CCM patient cohort was 75 years, and a majority (63%) were female. A significant proportion (68%) of patients presented with six or more chronic conditions, highlighting the complexity of their healthcare needs. Over the study period, a total of 174,612 CCM episodes (patient months) were delivered, averaging 6.6 episodes per patient, demonstrating sustained engagement with the CCM program.
Table 2. Characteristics of Patients Receiving Chronic Care Management Services Using Study Platform Between January 1, 2018, and December 31, 2018
| Patients, n | 26,500 |
|---|---|
| Type of Residence, n | |
| Private Home or Senior Living | 25,346 (95.6) |
| Nursing Home | 1175 (4.4) |
| Age, y | |
| Mean (SD) | 75 (13) |
| Median (25th, 75th percentile) | 76 (68, 85) |
| Sex, n | |
| Male (%) | 9799 (37.0) |
| Female(%) | 16,701 (63.0) |
| Number of chronic conditions | |
| 2–5 chronic conditions, n (%) | 8474 (32.0) |
| ≥6 chronic conditions, n (%) | 18,032 (68.0) |
| CCM patient months | 174,612 |
| Number of CCM episodes | |
| Mean (SD) | 6.6 (3.9) |
| Range | 1 – 12 |
| Ambulatory status, n | |
| Ambulates without assistance (%) | 19,052 (71.9) |
| Ambulates with assistance or nonambulatory (%) | 7458 (28.1) |
| ACP or DNR instructions, n | |
| Present | 15,117 (57.0) |
| Absent | 11,404 (43.0) |
| Risk of hospitalization risk flag, n | |
| Low or Medium Risk (%) | 22,496 (84.8) |
| High Risk (%) | 4015 (15.1) |
| John Hopkins Falls Risk Assessment, n | |
| Low Risk (%) | 7813 (32.8) |
| Medium Risk (%) | 6375 (26.8) |
| High Risk (%) | 9600 (40.4) |
| Polypharmacy risk, n | |
| Low Risk (%) | 1123 (4.5) |
| Medium Risk (%) | 4216 (16.9) |
| High Risk (%) | 19,619 (78.6) |
| Gagne 1-year mortality risk (n = 20,965) | |
| Mean (SD) | 7.% (7%) |
| Range | 2%–47% |
| Flacker 1-year mortality risk (n = 796) | |
| Mean (SD) | 23% (15%) |
| Range | 7%–86% |
| Hospitalizations in 2018, n | 2679 |
| Number of hospitalizations in a year | |
| Mean | 0.13 (0.42) |
| Range | 0–6 |
| Hospitalization Ratea | 184 |
aHospitalization rate is expressed as number of hospital admissions per 1000 CCM patient months per year.
ACP, advance care plan; CCM, chronic care management; DNR, do not resuscitate; SD, standard deviation.
Risk assessments conducted through the CCM platform revealed that approximately 15% of patients were flagged as high risk for hospitalization, 40% were at high risk for falls, and nearly 80% were in the high-risk polypharmacy category. Notably, over half of the CCM population (57%) had an advance care plan or do-not-resuscitate (DNR) instructions documented, suggesting a proactive approach to end-of-life care planning within the program. During 2018, the cohort experienced 2679 hospital admissions, resulting in an overall hospitalization rate of 184 admissions per 1000 patient months per year. This rate is noteworthy when considering the high-risk nature of the population and underscores the potential for chronic care management programs to save money by mitigating hospitalizations.
Logistic Regression Analysis: Identifying Key Predictors
The logistic regression analysis, after accounting for missing data and outliers, included 4352 patient records. The final model retained seven significant predictors of hospitalization, explaining approximately 11% of the variance in hospitalization data (Nagelkerke R2 = 0.113). Several factors were found to be associated with an increased likelihood of hospitalization, including younger age, independent ambulation, nursing home residence, a higher number of CCM episodes, and a greater 12-month predicted mortality risk. Conversely, a lower likelihood of hospitalization was associated with low polypharmacy risk and low falls risk, as well as, surprisingly, being identified as high risk for hospitalization.
The 12-month mortality risk emerged as the strongest predictor, with patients having higher scores on the mortality index being over 17 times more likely to be hospitalized. Nursing home residents were also significantly more likely to be hospitalized compared to community-dwelling patients. Interestingly, patients flagged as high risk for hospitalization were less likely to be hospitalized, suggesting that the identification of high-risk status and subsequent interventions within the CCM program may have been effective in preventing hospital admissions. This finding is a key indicator of how chronic care management programs save money by proactively managing high-risk individuals.
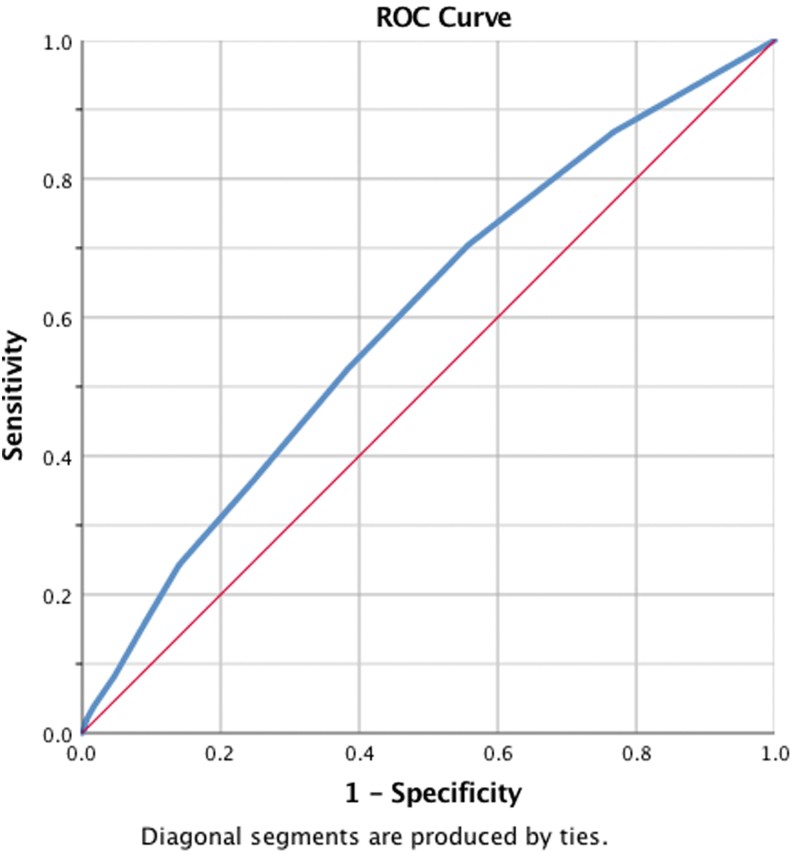
FIG. 3.
ROC curve for Gagne mortality risk index predicting hospitalization in community-dwelling CCM patients. CCM, chronic care management; ROC, receiver operating characteristic.
The ROC curve analysis for the 12-month mortality index (Figure 3) demonstrated moderate predictive utility for hospitalization risk (AUCROC = 0.60), indicating that this risk assessment tool, when integrated into CCM programs, can contribute to risk stratification and targeted interventions.
Further analysis focusing specifically on community-dwelling patients revealed an even stronger predictive effect of the Gagne mortality index, with a 32-fold increase in hospitalization risk for those with higher scores. This finding highlights the importance of mortality risk assessment in managing community-dwelling patients within CCM programs and further demonstrates how chronic care management programs save money by focusing on high-risk populations.
Discussion: Scalable CCM Model for Improved Outcomes and Cost Savings
This study provides valuable insights into the implementation and outcomes of a standardized, technology-enabled CCM program applied to a large cohort of 26,500 patients with multiple chronic conditions. The study population was characterized by a high burden of chronic illness and functional limitations, representing a patient group known to be among the most expensive within the Medicare system. The fact that over half of the cohort had advance care plans in place, significantly higher than national averages, suggests the CCM program’s success in promoting goal-directed care and proactive planning, which can contribute to both improved patient satisfaction and cost savings by aligning care with patient preferences and reducing unnecessary interventions.
The integration of evidence-based risk assessments into the CCM workflow proved effective in identifying and addressing key patient risks. For instance, the utilization of the OASIS risk of hospitalization assessment tool flagged 15% of patients as high risk. The proactive communication of this risk to the patient’s primary care practice, coupled with recommended interventions, may have contributed to the lower hospitalization rate observed in this high-risk group compared to those not identified as high risk. Similarly, the use of the John Hopkins Falls Risk Assessment (JHFRA) tool identified a substantial proportion of patients at high falls risk, providing actionable data to guide interventions aimed at falls prevention – a critical factor in reducing healthcare costs associated with falls and injuries.
The low overall hospitalization rate of 184 admissions per 1000 patient months per year observed in this CCM cohort is particularly noteworthy. While this study did not directly compare hospitalization rates to a non-CCM control group, the findings are consistent with previous research demonstrating the potential of CCM programs to reduce hospitalizations and associated healthcare expenditures. The logistic regression modeling further elucidated key factors associated with hospitalization risk, allowing for more targeted and personalized care management strategies. The strong predictive power of the mortality index, particularly the Gagne index in community-dwelling patients, underscores the importance of incorporating such risk stratification tools into CCM programs to identify and prioritize high-risk individuals for intensive support.
The counterintuitive finding that patients identified as high risk for hospitalization were actually less likely to be hospitalized suggests the effectiveness of the CCM program’s proactive interventions in mitigating hospitalization risk. This highlights the potential for chronic care management programs to save money by not only identifying high-risk patients but also actively managing their risks and preventing costly hospital admissions.
In conclusion, this study demonstrates that a technology-enabled, evidence-based CCM model is a scalable and effective approach to managing patients with multiple chronic conditions. By systematically identifying and addressing patient risks, these programs can contribute to improved patient outcomes and, importantly, significant healthcare cost savings. The findings strongly suggest that healthcare practices serving Medicare-age patients with multiple chronic conditions should consider implementing structured CCM programs, incorporating risk stratification tools like the Gagne mortality index, to optimize care and achieve both clinical and financial benefits. The care management strategies highlighted in this study have broad applicability within value-based care models, offering a promising path towards more effective and cost-efficient healthcare for complex patient populations.
Supplementary Material
Supplemental data: Supp_TableS1.pdf (22.8KB, pdf)
Author Disclosure Statement
The authors declared the following potential conflicts of interest: Dr. Mills, Mr. Douglas, Ms. Owens, Ms. Pridham, Ms. King, Ms. Roosa, Mr. Dznia, and Mr. Weber are employees of and stockholders in Chronic Care Management, Inc. None of these authors was involved with any aspect of the data analysis. All data and statistical analysis were performed by Dr. Poltavski, an independent statistician not affiliated with the company. Funding for this study was provided by Chronic Care Management, Inc.
Supplementary Material
References
(References are in the original article and should be preserved if needed for a full academic rewrite, but for SEO optimization and general audience, they may be less critical in the main body unless specifically requested.)
Associated Data
Supplementary Materials
Supplemental data: Supp_TableS1.pdf (22.8KB, pdf)