Millions of individuals across the United States grapple with serious illnesses, significantly impacting their quality of life and causing considerable symptom burden and caregiver stress. Palliative care, a specialized, team-based approach, has emerged as a crucial response to these unmet needs. It focuses on enhancing quality of life for patients and families facing serious illness, demonstrating improved outcomes and potentially lower costs compared to traditional hospital care models.
Building upon previous research indicating that 67% of U.S. hospitals with 50 or more beds offered palliative care programs by 2013, this analysis updates and broadens the understanding of palliative care program prevalence as of 2017. It investigates the hospital and market factors associated with the availability of these vital services. Comprehending the variations in palliative care program accessibility across U.S. hospitals is essential for improving care delivery to those with serious illnesses and their families. This article delves into the critical question: How Many Hospitals Have Palliative Care Programs and what factors influence their presence.
National Prevalence of Palliative Care Programs in Hospitals
A comprehensive cross-sectional study was conducted utilizing data from the 2017 American Hospital Association (AHA) Annual Survey Database™, supplemented with 2016 data for non-responding hospitals. This robust dataset allowed for a detailed examination of hospital-reported services, including inpatient palliative care. The AHA data was linked with demographic information from the United States Census Bureau’s 2017 American Community Survey and healthcare market data from the Dartmouth Atlas of Health Care to analyze geographic and socioeconomic factors.
The study focused on non-federal, general medical and surgical, children’s, cancer, heart, and obstetrics and gynecology hospitals with 50 or more beds within the 50 states and the District of Columbia. To ensure data accuracy, hospital palliative care program status from the AHA database was verified against the National Palliative Care Registry™, state-level directories, health system contacts, and web-based searches. Multivariable logistic regression models were then employed to identify associations between the presence of inpatient palliative care programs and various hospital, community, market, and geographic characteristics.
The findings revealed that 71.5% of the 2,409 U.S. hospitals included in the sample reported having palliative care programs. This translates to 1,723 hospitals offering these services in 2017. Consistent with earlier research, the study confirmed significant variations in palliative care availability based on hospital characteristics and geographic location.
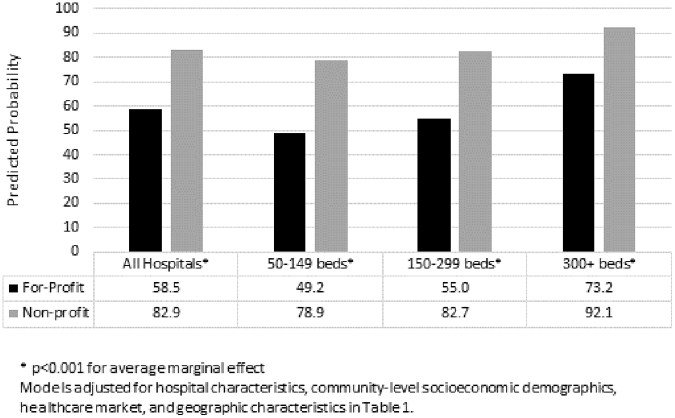
Figure 1: Predicted probability of a hospital having a palliative care program, categorized by hospital size and ownership type. Data reflects average marginal effects adjusted for hospital characteristics, socioeconomic demographics, healthcare market dynamics, and geographic factors as detailed in Table 1.
Key Factors Influencing Palliative Care Program Availability
Multivariable analysis highlighted several significant predictors of palliative care program presence. Hospital ownership emerged as a dominant factor, with nonprofit hospitals being 24.5 percentage points more likely to offer palliative care compared to for-profit hospitals (p<0.001). Geographic location also played a crucial role, as metropolitan areas showed a 15.4 percentage point higher likelihood of having palliative care programs than rural areas (p<0.05).
Table 1 further details these disparities, presenting a comprehensive breakdown of hospital characteristics associated with palliative care program availability.
Table 1. Characteristics of U.S. Hospitals with and without Palliative Care Programs (50+ Beds, 2017)
| Characteristics | Hospitals with palliative care (N=1723) % | Hospitals without palliative care (N=686) % | Adjusted Odds Ratio | 95% CI | p-value |
|---|---|---|---|---|---|
| Hospital Size | |||||
| 50–149 Beds (reference) | 51.1 | 48.9 | 1 | ||
| 150–299 Beds | 75.6 | 24.4 | 1.37 | 0.97–1.94 | 0.071 |
| 300+ Beds | 93.7 | 6.3 | 4.13 | 2.49–6.85 | <0.001 |
| Hospital Ownership | |||||
| For-profit (reference) | 34.7 | 65.3 | 1 | ||
| Nonprofit | 81.9 | 18.1 | 6.23 | 4.25–9.12 | <0.001 |
| Public | 60.0 | 40.0 | 4.41 | 2.64–7.38 | <0.001 |
| Teaching Status | |||||
| AAMC Member | 97.6 | 2.4 | 2.76 | 1.02–7.48 | 0.046 |
| ACGME Residency Program | 84.1 | 15.9 | 1.84 | 1.34–2.54 | <0.001 |
| ACS Cancer Program | 89.9 | 10.1 | 2.65 | 1.93–3.64 | <0.001 |
| Other Hospital Characteristics | |||||
| Catholic Church Operated | 90.5 | 9.5 | 2.91 | 1.75–4.83 | <0.001 |
| Hospice Program Presence | 80.2 | 19.8 | 2.24 | 1.63–3.09 | <0.001 |
| U.S. Census Region | |||||
| East South Central (reference) | 48.2 | 51.8 | 1 | ||
| New England | 92.3 | 7.7 | 3.12 | 1.09–8.93 | 0.034 |
| Mid Atlantic | 81.3 | 18.7 | 2.00 | 1.01–3.98 | 0.048 |
| East North Central | 82.1 | 17.9 | 2.28 | 1.20–4.35 | 0.012 |
| West North Central | 71.8 | 28.2 | 3.12 | 1.09–8.93 | 0.034 |
| West South Central | 50.5 | 49.5 | 2.00 | 1.01–3.98 | 0.048 |
| Pacific | 78.3 | 21.7 | 2.28 | 1.20–4.35 | 0.012 |
| Core-Based Statistical Area | |||||
| Rural (reference) | 17.3 | 82.7 | 1 | ||
| Urban | 79.3 | 20.7 | 3.52 | 1.19–10.36 | 0.023 |
| Community-Level Characteristics (Mean) | Hospitals with palliative care | Hospitals without palliative care | Adjusted Odds Ratio | 95% CI | p-value |
| Hospice Spending in HSA | $386.84 | $436.92 | 1.00 | 1.00–1.00 | 0.025 |
| Hospital-Based Physicians per 100k Residents in HSA | 25.2 | 24.5 | 0.96 | 0.93–0.99 | 0.024 |
| % County Graduating 4-Year College | 32.7% | 26.2% | 1.03 | 1.01–1.05 | 0.006 |
| % County 65+ Years Old | 14.9% | 15.7% | 1.05 | 1.00–1.11 | 0.048 |
Table 1: Detailed characteristics of U.S. hospitals with 50 or more beds, comparing those with and without palliative care programs in 2017. Data includes hospital size, ownership, teaching status, geographic region, and community-level demographics.
Other hospital characteristics significantly associated with palliative care programs included teaching status, presence of an American College of Surgeons-approved cancer program, Catholic church operation, and the presence of a hospice program. Conversely, for-profit ownership and rural location were strong negative predictors.
Implications and the Path Forward
This study reveals that while a significant majority (72%) of U.S. hospitals with 50 or more beds have palliative care programs, substantial disparities persist. The findings underscore that access to palliative care in U.S. hospitals is considerably influenced by both geographic location and hospital type. Despite the growth in palliative care availability since 2013, the identified disparities remain concerning. Notably, only approximately one-third of for-profit hospitals offer palliative care, and ownership-based differences are most pronounced in smaller hospitals. Although for-profit hospitals showed some growth in palliative care provision compared to 2013, they still lag significantly behind nonprofit and public hospitals. Regional disparities also persist, with the west south-central region continuing to exhibit lower prevalence despite showing the largest regional growth since 2013.
Several factors may contribute to these variations in palliative care program availability, including workforce limitations, inadequate financial incentives, a lack of accountability for palliative care access, and persistent knowledge gaps about palliative care’s benefits. It is crucial to recognize that this study only assessed the presence of programs and did not evaluate program quality, scope of services, or staffing levels, all of which are known to vary widely.
These findings emphasize the urgent need for targeted strategies to bridge the gaps in hospital palliative care availability across the nation. Ensuring equitable and reliable access to quality palliative care is paramount to meeting the needs of the millions of Americans living with serious illnesses and their families. Future efforts should focus on addressing the identified barriers and promoting the expansion of palliative care programs, particularly in underserved areas and within for-profit hospital systems, to ensure that all patients have access to this essential service.
Funding Information: This research was supported by grants from the Gordon and Betty Moore Foundation, the National Institute on Aging (Grant Number AG060270), and the National Palliative Care Research Center.
Author Disclosure Statement: The authors declare no competing financial interests.
References: (References from the original article would be listed here in a full publication, but are not included in the provided abstract excerpt.)